A bright spark fixing the electrics behind gut misery
30 January 2024
One student's success in the search for a link between unexplained gut misery and the electrical pulses in our stomach.
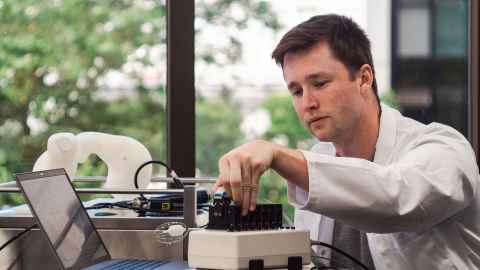
When Auckland Bioengineering Institute PhD student Peter Tremain headed back to Palmerston North for Christmas, he wasn’t planning to be lounging on the couch eating pavlova; he was going to be helping construct his parents’ new home.
The 26-year-old comes from a line of builders – and tinkerers; people who would choose to make something rather than buy it, he says. It’s what took Tremain – an academic kid and a good sportsman – into engineering in the first place. It seemed a practical profession; “something that gave me the technical skills I need to do sort of everything, to go in a lot of different directions”.
He was right. His early-stage engineering path has seen him shift from working for a start-up consultancy designing earthquake strengthening systems, to a PhD measuring the electrical pulses in the human gut as a way to diagnose and hopefully treat stomach problems.

Meanwhile, Tremain has been going in different directions geographically too.
In May, a travel award took him to Chicago for the Digestive Disease Week conference, the biggest annual clinical meet-up in the gut field. In August, he travelled to Silicon Valley as part of the University of Auckland’s Vanguard entrepreneurial leadership programme, funded by philanthropist Tony Falkenstein. And in early November, another travel award took him to Kobe for Japan Digestive Disease Week.
To cap off a stellar year came the announcement just before Christmas that Tremain had won a Prime Minister’s Scholarship for Latin America. This $10,000 award will fund a 12-week research collaboration with the Millennium Institute for Intelligent Healthcare Engineering in Chile later this year.
The Chilean institute is focused on developing medical imaging technologies integrating physics, engineering, and artificial intelligence. That’s a good fit with what Tremain’s team is doing at the Auckland Bioengineering Institute: developing a probe-style device which can be sent into the gut through the mouth.
In the same way an endoscope (a camera at the end of a long, flexible tube) might go into the body to take pictures, the ABI-developed probe is used to measure the electrical signals in the gut.
Imagine a deflatable Christmas bauble on the end of a tube. Where the outside of the bauble would be, is a skeleton made up of 64 electrodes.
When it’s flattened, it can go down the throat into the digestive system; once inside the body and inflated, the electrodes measure the pattern of electricity in the stomach and feed back data so doctors can work out whether that pattern is normal or not.

Scientists have known for a long time there is electrical activity in the body, but most of the early research was focused on the heart. Scientists realised in the 1800s it was electrical signals which told the heart to beat; it’s that electricity being measured (via electrodes stuck onto someone’s chest) by every ECG (electrocardiogram) machine you hear beeping in every hospital show on TV.
(Fun fact: ECGs at the very beginning of the twentieth century involved patients putting two hands and one foot in a bucket with electrolyte solution.)
Treatment for heart ‘arrhythmias’ – abnormal electrical heart signals – are pretty mainstream these days and include ‘ablation’, where tissue causing the abnormal electrical signals is destroyed, so it can no longer send those faulty signals to the rest of the heart.
But other organ systems use electric signals too - from the brain to the uterus.
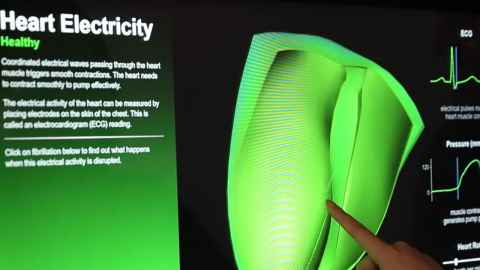
In the gut, it’s electrical pulses which stimulate the muscle contractions which move food through the different parts of the digestive tract. Even if you are upside down, your food will still move inexorably from mouth to anus.
Except, like in the heart, when the system stops working properly. Gut researchers at the Auckland Bioengineering Institute (ABI) have shown that electrical signals going awry – including going in the wrong direction – can be one reason for otherwise unexplained stomach symptoms like pain, nausea and vomiting, diarrhoea, bloating and wind.
The problem for doctors and researchers is that gut electricity is weaker than cardiac electricity, and the way it works is far more complicated. There isn’t a steady beat like in the heart, and different parts of the alimentary canal have different bio-electrical activity.
Scientists in the Auckland Bioengineeing Institute’s gastroenterology team are still working on understanding the link between abnormal gut electrical signals and people with stomach problems – and what to do about it. A different group is exploring whether ablation – the burning or freezing technique used in the heart to block irregular electrical signals – could be used endoscopically in the gut.
A poor cousin
Getting funding for gut research can be a challenge, says Dr Tim Angeli-Gordon, head of the TARGET Lab (Transitional Research in Gastroenterology and Emerging Technologies). Living with stomach problems will make your life wretched; endless pain, nausea, and diarrhoea can be debilitating and life-altering. But these symptoms are rarely life-threatening.
And often the big funding goes to the high-profile killer diseases (heart or brain problems, or cancer, for example), not the hard-to-diagnose, embarrassing, far-from-sexy, misery-causing gastrointestinal problems.

Tremain’s successes in the lab help bring a solution closer, Angeli-Gordon says. His scholarships, travel to overseas conferences, and stints with other institutions help bring the ABI’s gut work into the light – and hopefully into the dollars.
“Peter is a great combination of being intelligent, hard-working and determined, but also willing to put himself out there and take a bit of a risk.”
A tall poppy mentality in the New Zealand science community can mean people are hesitant to acknowledge their successes, and the importance of the work they are doing, he says.
“Telling people about what we are doing is as important as doing the research. If you don’t tell people about it, it’s difficult to have impact.
“What Peter’s been really good at is showing the impact of what we are doing, and the need for it – delivering new diagnostic and treatment options for patients, particularly disenfranchised patients.”
'My stomach hurts'
Gut problems can be super-hard to diagnose, Angeli-Gordon says. A patient might go to see their GP. “They say ‘my stomach hurts’, and their doctor says ‘what does it feel like?’, and they say ‘it hurts’ and the doctor says ‘where does it hurt?’, and they say ‘in my stomach’.”
There are only a handful of symptoms, and this handful of symptoms could point to a raft of different problems, Angeli-Gordon says. Although existing tests can diagnose many of them, others remain elusive.
In that case, one option for a clinician is to prescribe drugs which treat symptoms, not the underlying disease - and these drugs can come with unpleasant side effects. Or doctors can opt for a surgical approach, but that can sometimes drastically alter someone’s normal lifestyle.
Telling people about what we are doing is as important as doing the research; if you don’t tell people about it, it’s difficult to have impact.
“One of the exciting things with Peter’s project is that he’s running the first in-human trial and we’ve found we are able to record electrical activity of the stomach with our new endoscopic gastric electrical mapping device,” Angeli-Gordon says.
“Then with the data we can determine whether electrical rhythm is normal or abnormal.
“We don’t ultimately know what’s causing an abnormal rhythm – that's the next step. But it’s hugely valuable to be able to tell a patient this is occurring; it gives us a biomarker; something we can measure from your body to say there’s something wrong.”
Adding the Chilean factor
Tremain’s stint working with the Millenium Institute for Intelligent Healthcare Engineering institute in Chile later this year will be mostly focussed on two areas: ‘signal processing’ (interpreting the data delivered by the probe), and taking the device itself closer to a workable – and marketable – product, he says.
“The raw signals you get back from the device can be quite messy. So there’s a lot of hardware filtering you have to apply to it, and then a lot of signal filtering – cutting out certain frequencies and smoothing the signal so you can pick out what you need.
“For example, you’ll get cardiac signals mixed in there, or noise from breathing or movement – maybe a cable getting shifted or someone walking too heavily around the room – and you’ve got to filter all that stuff out.”
The second focus for Tremain's Chilean trip is getting help and spending time gearing up for the next stage of the process – commercialising the new gut electrode device.
Earlier this month, the team received just under $80,000 in a Ministry of Business, Innovation and Employment-funded medtech research acceleration grant to help with the next 12 months’ work redesigning and improving the device, Tremain says.
The Research Acceleration Programme is hosted by the University of Auckland on behalf of partners in the medtech research and medical device technology sector.
He’s putting himself out there, and that’s challenging; there’s potential for failure. Academia is riddled with rejection, but Peter and the rest of our excellent team have stuck with it.
Tremain and the other researchers in the Auckland Bioengineering Institute team have started initial scoping with UniServices, the University of Auckland’s commercialisation arm.
“I think we are at the pointy end where we have to figure out the best way of commercialising it. Early this year we’ll dive into that a bit more.”
Tremain’s Vanguard Entrepreneurial Leaders expedition to San Francisco included site visits to Amazon and Plug & Play, a high performance workshop hosted by Kiwi-co-founded coaching company Propel Performace, and a look behind the scenes at Synthego, a hot biotech that works with Crispr gene-editing technology.
“One of the most rewarding things has been seeing Peter achieve the success he has stepped out and strived for,” Angeli-Gordon says. “It’s not just about engineering or clinical work or device development; it’s also about the challenges of running a company.
“He’s putting himself out there, and that’s challenging; there’s potential for failure. Academia is riddled with rejection, but Peter and the rest of our excellent team have stuck with it.”
And the future?
“I feel we are on the precipice of a major breakthrough,” Angeli-Gordon says. “We are in clinical trials, we have a device that is minimally invasive, endoscopic, no surgery required. It’s relatively well-advanced in scientific terms – maybe five years away.
“We’ve shown that it works at an early level. Now we have to show what it’s capable of. And then? We want to get it into every hospital.”
Go to Mātātaki, The Challenge, for long-form stories and video on research and its impact.
For republication and media queries:
Nikki Mandow
E: nikki.mandow@auckland.ac.nz
M: 021 174 3142
Listen to Peter Tremain's interview with RNZ Nights' presenter Emile Donovan - The 26-year old breaking new ground on gut health