Getting to the guts of the electricity in our gut
01 December 2021
If cardiac pacemakers can correct abnormal heart rhythms through the application of electricity, could a similar technology be used to understand and potentially correct abnormal rhythms in the gut?
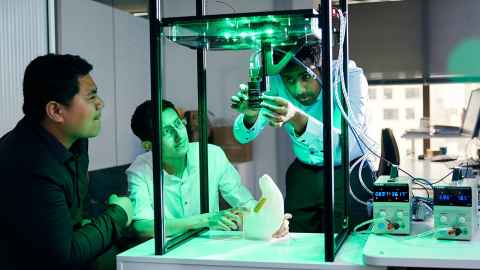
Dr Nira Paskaranandavadivel along with the team at Gastrointestinal Research Group at the Auckland Bioengineering Institute (ABI), has been researching the potential of electroceuticals in gut treatment for several years and has recently been awarded $900,000 from the Marsden Fund to further their investigations.
Electroceuticals have a long history in medicine, particularly for heart treatment, and increasingly, for the brain, such as with deep-brain stimulation for epilepsy and Parkinson’s disease. Dr Paskaranandavadivel’s research is aimed at investigating the potential of the technology in relation to the gastrointestinal (GI) system.
It is well known that that our cardiac system depends on bio-electrical signals, and when those signals go awry, they can be corrected with electroceuticals - technologies that treat ailments with electrical impulses.
“And it has been known for 100 years that the gastrointestinal system is also governed by bio-electrical activity, but that bio-electrical activity is not as well understood, and consequentially, there are limited treatments available for disorders that affect it,” says Dr Paskaranandavadivel.
Gut disorders have typically received less attention because they tend to be chronic and less severe than, for instance, heart disease – they won’t kill us, but they can make life very difficult for many.
“But there is a renewed interest in understanding the gut and how bio-electricity is used to control function,” he says.
The network of neurons lining our gut is so extensive that scientists have nicknamed it our "second brain”. It is affected by hormones, by the food we eat and psychological issues - many of us will be familiar with the flight or fight response in the gut if, for example, we are asked to speak in front of an audience.
One of the key issues is that the gastrointestinal system is extremely complex. The network of neurons lining our gut is so extensive that scientists have nicknamed it our "second brain”, it is affected by hormones, by the food we eat and psychological issues - many of us will be familiar with the flight or fight response in the gut if, for example, we are asked to speak in front of an audience.
The Marsden funding will allow him and his team to use electroceuticals to better understand the mechanisms underlying peristalsis. This is the involuntary constriction and relaxation of the intestinal muscles upon which digestion and nutrition depends.
They will be using electroceuticals in combination with multi-modal high-resolution imaging methods and couple the data gathered from that with multi-scale modelling techniques – using mathematical modelling to identify how the behaviour of cells, tissues and the organ system affects each other. (The approach is similar to methods used in Covid modelling and in the engineering of America’s Cup boats.)
“This will allow us to simulate biological system response to an electrical activity, and how that affects motor function,” he says. “We’re trying to break the GI system into singular units, to understand if, for instance, when we use electrical stimulation on the organ, how does that react with the cell or tissue, how does that affect the motor function.”
Multi-scale mathematical modelling allows researchers to investigate how the gut works and potential treatments, without relying solely on animal or human experiments he says. “With electroceuticals we’re delivering external energy, and so we need to be careful about safety; we first need to develop the correct models, to understand, with precision, the effects of that input.”
“Mathematical modelling is increasingly used in biology and medicine, as an acceptable way of testing to understand biological and physiological principles, and increasingly, in the approval process for medical devices, and for clinical decision making. We aim to use this to accelerate our understanding of peristalsis in the gut.”
The project team includes both ABI researchers (Professor Leo Cheng, Associate Professor Peng Du and Dr Recep Avci) and renowned international researcher, Professor Jack Rogers, University of Alabama.
“Our research will help identify mechanisms for peristalsis which in turn will guide the use of electroceuticals to understand the electrophysiological basis of gut disorders, and ultimately, to offer more effective tools for both the diagnosis and treatment for those disorders.”
Media contact
Margo White I Media adviser
DDI 09 923 5504
Mob 021 926 408
Email margo.white@auckland.ac.nz