Real life tricorder screens skin cancers
21 April 2020
More New Zealanders die from skin cancers than on our roads each year. A real 'tricorder' aims to cut that death toll.



A Star Trek-style laser device to scan people for skin cancer is on the brink of becoming a reality, suggesting a breakthrough in tackling New Zealand’s world-leading rates of the disease.
A prototype of the device could be ready within months, according to the scientist leading the project, Michel Nieuwoudt, of the University of Auckland’s Photon Factory, a research group applying the properties of light for energy, health and technology.
The device has the potential to slash New Zealand’s death rates from the disease and revolutionise the prevention and treatment of skin cancer worldwide by making diagnosis faster, more accurate and easier to access.
A quick scan could reveal whether a skin condition is, say, a basal cell carcinoma (BCC), the most common type of skin cancer, or a melanoma, the most serious type. Avoiding the months of delays from referrals and repeated biopsies will save lives. Patients whose blemishes are benign could forgo biopsies and scarring, avoiding the drain on resources from unnecessary procedures.
Science fiction fans will recall Bones McCoy in Star Trek scanning patients with a handheld computer to instantly diagnose members of the U.S.S. Enterprise who struck strife in alien lands. It sounds fanciful, but, for skin cancer, Nieuwoudt’s device, featuring a laser on a flexible probe, will turn science fiction into fact – quickly assessing moles, freckles and lesions to come up with a verdict of cancerous or benign.
The incidence rates in New Zealand and Australia are two times those observed in any other country. Over 90,000 New Zealanders are diagnosed with a skin cancer each year, more than the population of Palmerston North.
Over 90,000 New Zealanders may be diagnosed with skin cancer in a year – more than the population of Palmerston North. More than 500 people may die, exceeding the annual road toll. Melanoma incidence rates in New Zealand and Australia are two times those observed in any other countries. Māori and Pacific people are less likely than fair-skinned New Zealanders to be diagnosed with melanoma but their cancers when detected are more aggressive with a poorer prognosis.
"There’s a huge variation in accuracy of diagnosis of melanomas,” says Nieuwoudt, citing published studies. "A clinician’s accuracy varies between 30 and 95 percent depending on whether they’re a GP or a dermatologist.” She’s aiming for 99 percent accuracy.
Colonisation and migration led to Australia and New Zealand becoming the world’s worst countries for the disease because of the many people who arrived from cloudier climes, lacking protective pigmentation in their fair skin.
Adding to that, skin-damaging ultraviolet radiation from the sun runs at higher levels than in similar latitudes in the Northern Hemisphere because of cleaner air, a thinner ozone layer, and the countries’ proximity to the sun in summer. New Zealand’s always-nearby beaches and the country’s love of outdoor pursuits only add to the toll.
The shocking cost is brought home when Nieuwoudt and her team use a laser with a flexible probe to scan skin cancer patients who are about to undergo surgery in the William Manchester plastic surgery suite at Middlemore Hospital.
Greater good
Donning protective goggles because of the laser, patients donate a few minutes of their time to help build a database for the classification algorithms to be used in diagnosis. The team scan cancerous and pre-cancerous lesions selected by plastic surgeon Michelle Locke.
Patients treated for skin conditions such as eczema, psoriasis and the benign annular seborrheic keratosis at the Manukau SuperClinic are also scanned, and samples of normal moles are gathered via free skin checks offered to the public at the clinical research department of the University of Auckland Medical School. With no central global database of lesions to draw on, Michel’s team have so far assembled 2000 samples of skin conditions, from the healthy to the deadly.
The people who are scanned are very enthusiastic, according to Paul Jarrett, who’s a member of the team and a dermatologist at Middlemore Hospital. “They’ve very altruistic – they recognise it’s for the greater good.”
Imagine a doctor in a remote area plugging into a 4G or 5G network to tap a “database bigger than Texas” of skin conditions, and getting an answer virtually straight away, he enthuses.
For now, Nieuwoudt’s team is using a benchtop scanning device, about the size of a couple of loaves of bread. The key technique underpinning the scanner is Raman spectroscopy, named after Indian physicist and Nobel Prize winner C.V. Raman. Here reflected or scattered photons reveal information about the make-up of an object targeted by a laser light. Think of it as a torch that reveals what's inside things.
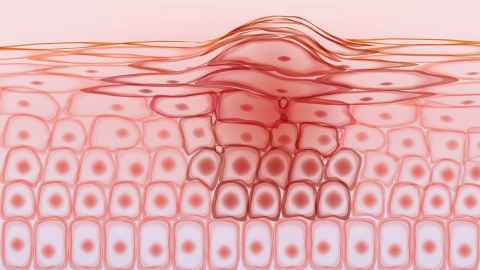
Nieuwoudt's would-be Star Trek device looks for clues such as the higher-than-normal levels of the amino acid tryptophan that indicate certain cancers. Changes in skin components such as collagen, fatty acids, elastin and melanin can also be indicators.
One of the biggest scientific challenges is that lasers used on human skin need to be low-powered, limiting the strength of the reflected signals available for analysis. It was around 2007 that the idea of using Raman spectroscopy to identify skin cancers surfaced internationally in scientific papers, Nieuwoudt recalls.
Watching the field, she couldn’t see anyone suggesting a device as good – or as small – as she envisaged. In 2017, the Ministry of Business, Innovation and Employment granted $1 million from the Endeavour Fund for her to pursue the project. With that funding set to run out at the end of 2020, the venture is now looking via investment firm Pacific Channel for investors to take the device through clinical tests and to market.
As of the start of 2020, her team includes plastic surgeon Michelle Locke and Paul Jarrett at Middlemore Hospital, Professor of Physics Cather Simpson, postdoctoral research fellow Hannah Holtkamp and PhD student and statistician Cannon Giglio.
"We’re trying to make it as affordable as possible because our aim is to enable rural clinics, and everybody to have one,” says Nieuwoudt.
“The price very much depends on the technology at the time. If you were buying a laser 10 years ago, you would be paying a crazy amount of money for it – now it’s much cheaper to get a small solid-state diode laser.” She can imagine an initial price tag in the $10,000 ballpark. For now, the device is geared to clinicians, but one day it could be sold to the public.
Story by Paul Panckhurst
The Challenge is a continuing series from the University of Auckland about
how our researchers are helping to tackle some of the world's biggest challenges.
To republish this article please contact: gilbert.wong@auckland.ac.nz