How the PCR test works and why it’s such a critical weapon against Covid-19
21 September 2020
Opinion: Misinformation about the effectiveness of the polymerase chain reaction test is swirling, but in fact the PCR is both reliable and critical in taking on the virus, explains Associate Professor Siouxsie Wiles.
I’ve been asked by several people in recent days whether there is any truth to a video about the Covid-19 PCR test that is currently doing the rounds on social media. I’m not linking to it, because it is chock full of false information; the fewer people who see it the better. It is by a medical doctor who talks about the difference between diagnostic and screening tests. She sounds like she knows what she’s talking about so I can see why people are confused.
Before I get into what the current Covid-19 tests can and can’t tell us, what I will say is that just because someone is medically qualified doesn’t necessarily mean they know anything about diagnostic testing and the intricacies of quantitative PCR (polymerase chain reaction). The same goes for epidemiologists, engineers, and low-carb diet advocates. It’s also worth remembering that there are people who are actively trying to make everyone lose confidence in the PCR tests in order to push the idea that Covid-19 can’t be managed and we just need to learn to “live with the virus”.
Testing for the virus
I’ve written before about the hundreds of tests for Covid-19 that are either in development or already commercially available. Some of them test for the presence of the virus. Others test for our body’s response to the virus. In that same piece I also wrote about the Foundation for Innovative New Diagnostics which has offered to put the tests through their paces. They’re making their findings available for anyone to look at.
Like us, the SARS-CoV-2 virus responsible for Covid-19 has a set of genetic instructions called its genome. While we might not know exactly what each gene in that genome does, we do know that together they make up the virus. The PCR test looks for specific genetic sequences that are only found in the SARS-CoV-2 virus. That makes it very suitable as a screening tool as it has such a low false-positive rate – people are highly unlikely to test positive unless the virus is present in the sample. We know this is true from all the thousands of negative tests we’ve seen here in New Zealand.
We also know the PCR tests really do detect viral sequences as this has been confirmed time and time again by also sequencing the entire viral genome from a positive sample. In New Zealand we’re now using genome sequencing as an extra bit of information to see which cases are linked together. This can help to define a cluster or even understand how someone might have become infected as happened in with the Rydges maintenance worker or the recent community case in a person who had tested negative while in managed isolation.
The ‘sensitivity’ of the PCR test
According to the Foundation for Innovative New Diagnostics’ dashboard there are now hundreds of versions of the PCR test. What differentiates them is the equipment they are designed to run on and the specific genetic sequences they look for. Some of the test kits can detect as few as 1-10 copies of the specific viral gene they are designed to pick up. That makes them super-sensitive.
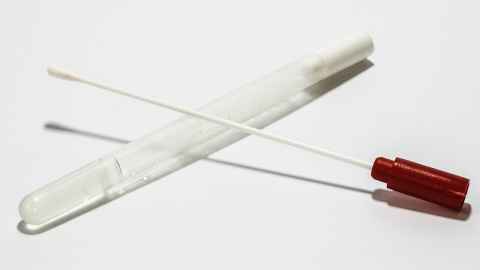
Despite this, you might have seen people claim that PCR testing only has a sensitivity of 60-70%. I’m not quite sure where that number has come from or what they actually mean by it, but I think they might be trying to quantify how many infected people would wrongly test negative by the PCR test. The reality is that while the test itself is very sensitive, the way we are using it in New Zealand and in many other places around the world requires someone to have a swab stuck right up to the back of their nose. This is where things can get a bit tricky, because depending on how well the swab is inserted and moved around, it’s possible to not get enough genetic material for the PCR test. And that could mean an infected person tests negative. That’s why it’s utterly farcical that some countries tried to roll out home-swabbing kits in an effort to improve their testing capacity. Do you think you could swab yourself properly? Maybe the medical professionals among us could but I’m pretty sure I couldn’t.
The good news is things have moved on. Dr Anne Wyllie is a New Zealand scientist at the Yale School of Public Health in the US. She led a team that has developed a method for testing saliva for the virus instead of using swabs to collect a sample. Spitting into a container sounds much easier. Not only was it easier, but it also picked up people who had tested negative by nasal swab. The US Food and Drug Administration have granted the method an emergency authorisation so it can be used to test people. I’m told ESR is looking into using the method here in New Zealand. I really hope they do as it would be a much more palatable way to test people, especially those who work at the border or in managed isolation and quarantine and need to be tested regularly.
The PCR test captures a moment in time
The most crucial thing to understand about the PCR test is that it is basically us asking: was the virus present in sufficient quantities to detect when the person was tested? Let’s recap what happens after someone is exposed to the virus. First, they enter what is called the incubation period. This is the time between exposure and when symptoms develop. This period can be as short as one day or as many as 20 or so. The overwhelming majority of people develop symptoms within 14 days. About one in 100 may develop symptoms after 14 days but most develop symptoms within two to 10 days. Those symptoms range from unnoticeable to mild to deadly. Some people may not develop any symptoms at all. At some point infected people become infectious themselves. This is how the virus spreads, exponentially if we don’t put any measures in place. I’m still not sure we know for certain just how infectious people who never develop symptoms are. The best study I’ve seen was from a while ago and it was small compared to how big the pandemic is now but those people who did not develop symptoms didn’t spread the virus to anyone else.
As for those who do develop symptoms, what we know is that they will be infectious for a few days before their symptoms appear and for the first few days that they have symptoms. This is the time in which we need to act to minimise and preferably stop the virus spreading further. So what’s happening with virus levels during this time? Well, it will differ between people. On average, though, virus levels start rising at some point during the incubation period as the host’s cells are turned into little virus-producing factories. Levels then peak around when people start to develop symptoms and fall as the person’s immune system kicks in to get rid of the virus. Once that’s happened, they may be left with bits of viral debris floating around.
PCR cycles and ct values
Many of the PCR tests available for the virus use a method known as quantitative PCR. The more virus or bits of virus present in the original sample, the quicker the test becomes positive. You might have heard people talk of ct (cycle threshold) values and cycles. These are measures of how quickly a sample tests positive. The higher the ct value or number of cycles, the lower the levels of virus present. A “weakly” positive test result will be one with a high ct value and may be from someone very early on in the incubation period where the virus hasn’t quite got started yet, or later once they are no longer infectious and all that’s left is viral debris.
So, to summarise. The PCR test captures a point in time. People can test negative and still actually be infected, just inside the incubation period.
That’s why if someone is considered a close contact, they still have to isolate for fourteen days, even if they test negative. And why they should keep an eye out for symptoms after 14 days, just in case they are a long incubator. People can also test positive but not be infectious anymore. Those looking at the test results will be able to use the ct value to help decide what advice to give the person testing positive about whether they need to continue isolating or not.
Why test at all?
I’ve heard people say that because the PCR test has limitations it’s not worth testing people. I strongly disagree. It’s important to know who has been infected to learn more about the epidemiology of the pandemic and the potential long-term consequences of the virus. But more than that, testing is a crucial part of the test-trace-isolate strategy for stopping transmission of the virus.
For the strategy to be successful, people need access to testing as soon as they develop symptoms, and for test results to come back within a day or two. That allows the contact tracers to swing into action, identifying everyone the infected person had contact with while they were infectious, and getting those people into isolation if necessary. That stops further spread of the virus. If it takes more than a few days for test results to come back, then you lose the window for isolating both the infectious person and their close contacts and the virus makes another move down the transmission chain.
Of course, the test-trace-isolate strategy also needs to have good contact tracing capacity, and people need to understand the importance of isolation and have the means to do so. In Taiwan, people are paid an allowance when they have to self-isolate and have to pay a huge amount back if they fail to do so.
Around the world countries are grappling with how to deal with the pandemic. This is clearly a difficult virus. People are infectious before they have symptoms, and many of the symptoms mimic other infections and health conditions. Those are not reasons to quit trying to prevent the virus from spreading. The PCR test is a valuable part of our toolkit to do this and it’s working really well in New Zealand.
Associate Professor Siouxsie Wiles is a microbiologist from the Department of Molecular Medicine and Pathology in the Faculty of Medical and Health Sciences' School of Medical Sciences.
This article reflects the opinion of the author and not necessarily the views of the University of Auckland.
Used with permission from The Spinoff, How the PCR test works and why it’s such a critical weapon against Covid-19, 21 September 2020.
Media contact
Paul Panckhurst | Media Adviser
Mobile: 022 032 8475
Email: paul.panckhurst@auckland.ac.nz