We must change tack on ‘racist’ disease
22 January 2021
Opinion: Our approach so far to end a 'racist' disease – acute rheumatic fever - has not worked for all. It's time to try something new, writes Collin Tukuitonga.

Acute rheumatic fever and the rheumatic heart disease it causes, long-known as a disease of poverty, is a blight on the wealth and prosperity of Aotearoa New Zealand. It is a symptom of the uneven distribution of power and resources in our supposedly egalitarian country.
As we move into a new year, albeit with Covid still rampant across the world and global politics causing unease and worry, surely it is time to look closer to home and find a new approach that will work for all to end this third world ‘racist disease’ that shames our nation.
I use the term ‘racist disease’ because acute rheumatic fever is endemic mostly in Māori and Pacific communities. It affects mainly the young, aged between five and 14 who live in cold, damp, overcrowded housing with poor access to health care and can mean a lifetime of poor health and missed opportunities. For some of our young men, it can mean the end of a promising rugby career and a potential path to economic independence. For their families, it can mean a lifetime of dealing with a monocultural and unresponsive health system.
It would be hard to find a more powerful statement against social, economic and cultural determinants of health in Aotearoa New Zealand. It is regularly described as the ‘canary in the mine’ for many other health inequities we have in this country.
The present Government has shown good intent to address this issue. The Labour Party’s 2020 election manifesto included an allocation of $55 million over four years to rid the country of this disease which the Prime Minister herself has described as a "national shame".
Most of this money will go to the Healthy Homes Initiative to tackle poor quality housing, which we know is significant to the development of rheumatic fever. This initiative sets minimum standards for heating, insulation, ventilation, moisture and drainage across the country.
It sounds promising. It's a sizeable budget and the Government has included additional funds to ensure rental accommodation meets the same standards. But will it work for all? Previous government programmes to prevent ARF and RHD have had little impact on Pacific families.
For example, a decade ago the Ministry of Health set up the Rheumatic Fever Prevention Programme (RFPP). Initially, this programme focused on the prevention and treatment of sore throats, which are linked to the development of rheumatic fever.
The following year, in 2012, the government invested a further $65 million to expand the programme to meet newly introduced five-year rheumatic fever Better Public Services target. This target aimed to reduce rheumatic fever by two-thirds to 1.4 cases per 100,000 people between 2012 and June 2017.
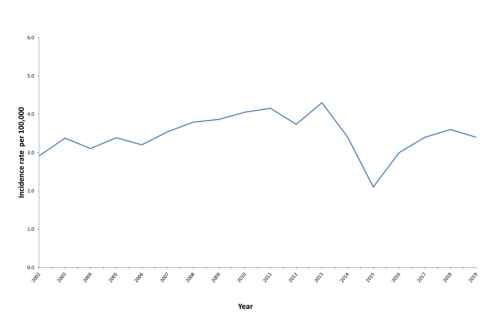
Was it effective? The graph below (from the Ministry of Health website) shows the rate of Māori and Pacific people admitted to hospital with rheumatic fever for the first time between 2009 and 2019.
The good news indicated by the statistics used here is that, by 2019, the rates of rheumatic fever in Māori communities had reduced by 30 percent compared with 2012. Unfortunately, the Ministry’s statistics show rates for Pacific people had increased by 2019 compared to pre-2012.
So maybe it’s time to reconsider the approach for Pasifika? Maybe it’s time to look at giving Pacific families, communities and health workers ownership of decisions around ARF and RHD prevention. Perhaps, by owning the challenges and leading the changes, those families and communities most affected by these diseases can make a difference.
This may sound like speculation, but the statistics show clearly that we need a new approach. Informed and engaged communities are empowered communities; and empowered communities can be the most powerful innovation we have to address the ongoing scourge of ARF and RHD.
Dr Collin Tukuitonga is the inaugural Associate Dean Pacific in the Faculty of Medical and Health Sciences.
This article reflects the opinion of the author and not necessarily the views of the University of Auckland.
Used with permission from Newsroom We must change tack on ‘racist’ disease 22 January 2021.
Media queries
Alison Sims | Research Communications Editor
DDI 09 923 4953
Mob 021 249 0089
Email alison.sims@auckland.ac.nz