Sweet pressure – scientists discover link between high blood pressure and diabetes
02 February 2022
Scientists are preparing to test a novel medication on patients with a potentially fatal combination of high blood sugar and high blood pressure.

Scientists at the universities of Auckland and Bristol are preparing to test a novel medication on patients with a potentially fatal combination of high blood sugar and high blood pressure, after promising findings in animal studies.
The team of international collaborators has just had their findings published in preeminent scientific journal Circulation Research.
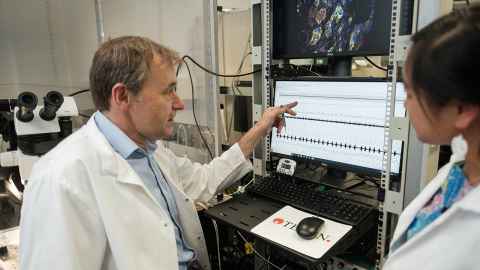
Professor Julian Paton, the senior author and director of Manaaki Manawa, the Centre of Research at the University of Auckland says: “We’ve known for a long time that hypertension and diabetes are inextricably linked and have finally discovered the reason, which will now inform new treatment strategies.”
Around one in four people will experience high blood pressure at some time in their life, but despite it being so common, it is poorly controlled in half of those people. Meanwhile, Aotearoa New Zealand has some of the worst statistics for diabetes in the world.
Two-thirds of people with diabetes will also have high blood pressure (hypertension).
“Another problem we have, clinically, is trying to lower blood pressure in patients with high blood sugar, diabetes; it is very much more challenging than if the patient just has high blood pressure alone, which tells you there's a different mechanism,” Professor Paton says.
The international team has demonstrated that a small protein called glucagon-like peptide-1 (GLP-1), which was already known to regulate insulin, also controls blood pressure via the nervous system – a novel finding.
“Locating the link required genetic profiling and multiple steps of validation; we never expected to see GLP-1 come up on the radar, so this is very exciting and opens many new opportunities,” says Professor David Murphy from the University of Bristol.
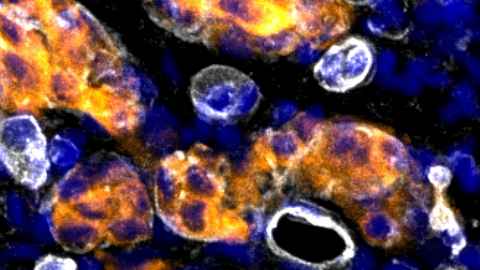
GLP-1 is released from the wall of the gut after eating and acts to stimulate insulin from the pancreas to control blood sugar levels. GLP-1 also stimulates a small sensory organ called the carotid body located in the neck.
“The carotid body is the convergent point where GLP-1 acts to control both blood sugar and blood pressure simultaneously; this is coordinated by the nervous system which is instructed by the carotid body,” Professor Paton says.
“What we found, in an animal model, was high blood pressure and metabolic disturbance, which means glucose control problems or diabetes, is that the GLP-1 signalling pathway is disrupted. The carotid body has become desensitised to glucagon-like peptide-one (GLP-1) and this leads to high blood pressure and high blood glucose,” Professor Paton explains.
People with hypertension and/or diabetes are at high risk of life-threatening cardiovascular disease. Even when receiving medication a large number of patients will remain at high risk of cardiovascular disease. This is because most medications treat symptoms and not the real causes of high blood pressure and sugar.
“We've found a common mechanism, which we've been looking for, for years. Linking diabetes and hypertension,” Professor Paton says.
“GLP-1 could now be considered in patients with high blood sugar and blood pressure and be given solely or in combination with existing medications,” he says.
Professor Rod Jackson, an internationally leading epidemiologist at the University of Auckland says, “We’ve know that blood pressure is notoriously difficult to control in patients with high blood sugar, so these findings are really important because by giving GLP-1 we will be able to reduce both sugar and pressure together, and these two factors are major contributors to cardiovascular risk.”
The prevalence of diabetes and hypertension within our communities is some of the worst in the
world.
“These findings may provide a new way to control the tsunami of diabetic hypertensive patients we face in Aotearoa and offer us a natural form of treatment because GLP-1 is produced by our body,” Professor Paton says.
The next step will be to seek ethical approval trial the naturally occurring compound on patients with diabetes and hypertension at Auckland Hospital.
“We've done some preliminary work in in humans. We know that the signalling pathways is the same. So what we would like to do next is set up a clinical trial with diabetic, hypertensive patients,” Professor Paton says.
The study was funded by the Health Research Council of New Zealand and the British Heart
Foundation.