Advanced AI set to teach clinicians empathy
7 October 2022
AI will be used to train medical and other health students to be more empathetic and patient-focussed, as a result of a University of Auckland research project.

Conversational AI is being used to build virtual patients that will teach medical students how to be empathetic, as part of a University of Auckland research project.
An empathetic consultation is one where the clinician validates the patient’s feelings and develops a treatment plan in partnership with the patient, informed by their individual experiences.
“Empathy leads to better outcomes for the patient, better adherence to the treatment plan. It also reduces stress and burnout for healthcare professionals and improves their job satisfaction,” doctoral candidate Monika Byrne says.
Byrne is currently reviewing existing research and developing the training programme, using a model of empathy with elements that can be taught and assessed.
The healthcare professional doesn’t necessarily need to feel the emotions with the patients, a ‘shortcut’ is to respond cognitively by thinking “I know what that feels like.”
“I think the way empathy works is we learn throughout life how things feel in our bodies,” Byrne says. “Then we build this cognitive library of human experiences and emotions that go with them - what it’s actually like to be in emotional pain, for example, to lose a partner or to fail.
“We don’t necessarily have to feel it in our own bodies in a given moment to exhibit empathy, but we need to have experienced something like it before. So, we have this cognitive library that builds out of these experiences.”
Byrne is also describing subskills involved in empathetic consults, such as an ability to focus attention and to self-regulate.
Scientists at the University of Florida’s Virtual Experiences Research Group are assisting Byrne to build virtual patients that can converse and express feelings, a technical challenge.
The Florida researchers have been building virtual patients for around two decades.
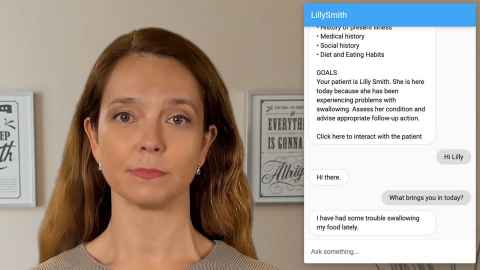
They appear, as avatars, on a screen and the student can chat with them using a chat function.
Byrne intends to adapt five of their virtual patients for this project to make them suitable for empathy training - give them ability to talk about and express emotions and preferences and ask questions.
Using AI will not replace the need to train with actors or real patients but will give students ability to practise engaging with empathy before their clinical placements, save universities money compared with using actors and be engaging for students through gamifying learning.
Another goal is for the virtual patients to be able to express difficult emotions, such as anger and distress. Plus, they will need to teach students how to relate empathetically to people who are very different to themselves, including culturally.
Byrne has completed masters degrees in English (University of Warsaw), Computer Science (University of Westminster) and Bioinformatics (University of London) and has worked as a software engineer and IT systems/business analyst in the pharma industry and academia.
Most recently Byrne completed a masters degree in Bioengineering with the Pregnancy Health group at the Auckland Bioengineering Institute. This involved developing a computational model of feto-placental circulation based on micro-CT images of a delivered placenta.
After considering a doctorate in that area, she was attracted to this research project because of her own experiences as a patient of a lack of empathy.
“I thought that’s something that’s close to me and that I care about. I really want to improve that experience for other patients,” Byrne says.
Now Byrne is collaborating with the University of Auckland’s Speech Science department and its Centre for Medical and Health Science Education.
Her plan is to run pilots and get feedback as she develops the AI before conducting a randomised, controlled trial and publishing the results.
Media queries
FMHS media adviser Jodi Yeats
M: 027 202 6372
E: jodi.yeats@auckland.ac.nz