Rural placement pivotal experience for pharmacy student
12 June 2025
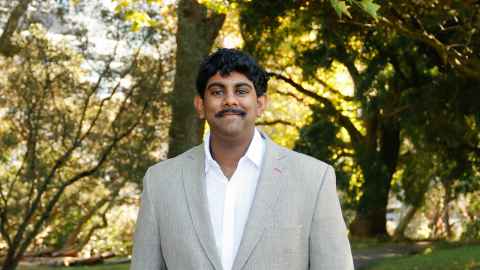
Pharmacy student Sendhil Rungasamy will ‘only plans on working in rural’ now, after a rural interprofessional training placement changed his view of healthcare.

Pharmacy Today: A rural location is the only place fourth-year University of Auckland School of Pharmacy student Sendhil Rungasamy wants to work after doing his University's rural interprofessional placement.
Rungasamy recently came back from five weeks working at the Whakatāne Hospital dispensary pharmacy as part of the Rural Health Interprofessional Programme.
Started in 2012 by Te Whatu Ora Hauora a Toi Bay of Plenty and Waipapa Taumata Rau, University of Auckland, the Rural Health Interprofessional Programme sees undergraduate students from different health disciplines at several tertiary institutes gaining experience in rural clinical settings.
Over 600 students from 13 disciplines, including 70 pharmacy students, have completed the programme since its inception. Each cohort lives together, and they work in placements at both the hospital, primary care and community settings in Hokianga and Whakatāne.
The programme starts with a noho marae (a stay at a marae) to immerse participants in Māori health and to help them understand health inequities from tangata whenua.
Then come placements under the guidance of local healthcare professionals and academic staff, as well as outings to see local communities including Hauora Māori providers, kura (school) visits and police and fire-fighters.
“I went on the placement scared, and now I just need to go back and immerse myself in that environment again. It's honestly a blessing and a privilege to work with all these students who are from the same university as I am, but I'd never get the chance to work with [them] and meet otherwise,” Rungasamy, who was born in South Africa but grew up in Porirua, says.
“We all have different backgrounds but now have the same goal – to uplift different communities, uplift kaupapa Māori and to provide collaborative care.”
Firsthand experience of inequity
Seeing firsthand that healthcare is not readily available to people in a rural community is different to learning about disparities in health in a lecture theatre, Rungasamy says.
“On my first day in hospital meeting patients ... you realise there is not enough medication on hand and a medication is taking a while to come in – you really get to see and be in the thick of it and ask ‘why aren't we supporting them?’
“I’d talk to patients who'd been prescribed an inhaler but didn't know how to use it – I'd ask why, and they'd say, ‘I had a quick appointment with the doctor, but I had to get going as my place is two hours away – do you know how to use this?’”
There are not just mental and emotional barriers but physical barriers to accessing healthcare, Rungasamy says.
“In Auckland, if you break your leg, you can get a scan in two or three days ... Whakatāne Hospital doesn't have an MRI machine. So you have to wait for two to three weeks for a scan at Tauranga Hospital which is an hour-and-a-half’s drive away.”
Eastern Bay's Rural Health Interprofessional Programme student placement coordinator Nikki Wana says the programme has led to profound changes in participants' outlook, and how they practise, as well as helping form lifelong friendships.
In part, the programme aims to encourage students to work in rural areas once qualified, Wana explains, and it has some success at this, although exact figures were not available.
“We want to increase opportunities for the students – to expose students to developing an understanding of the different health needs of our rural communities versus the needs of our Māori communities. To offer integrative learning opportunities, and the chance to make lifelong friendships.”
Rungasamy says, after the experience, “I only plan on working in rural.”
Marae visit broadens outlook
The most recent Rural Health Interprofessional Programme cohort of 14 students from nine different health disciplines were hosted at Ōwhakatoro Marae, Rūātoki within the boundaries of Tūhoe, which is approximately a 71km return trip from Whakatāne.
“We’re aware that some of the students have never been to a marae – some of the students have never been outside of Auckland before. The hau kāinga addresses them and we take things at the students’ pace, with plenty of walks outside,” Wana says.
Often historical content is shared on these walks, with Rongoā Māori knowledge shared and historical landmarks visited.
One of the kuia who lives on the marae is one of four generations. She talked about Hauora Māori and Rongoā Māori, and on the impact on Māori who no longer have access to the sea or the land for kai – the adjustments still for Māori now living in Whakatāne town, not rurally,” Wana says.
"Over the five weeks you hear the students’ questions deepen in relation to their time spent here. They see the state of the roads we’re travelling on – they visit a kura just 20 minutes out of Whakatāne where the teachers take bottled water for their students because the school water tanks aren't up to standard,” Wana says.
Where rural areas lack resources, their strength lies in their community, Rungasamy says.
“Everyone wraps around each other. Whakatāne Hospital is a small hospital and everyone knows everyone, everyone can talk to everyone, and everyone feels free to say what they want to say, and everyone's opinion is validated and valued.
“In Auckland, you hear about cultural safety, but it feels like an option. In Whakatāne, it feels like a responsibility – treating individuals with humility and sharing power in the space where decisions are made,” he says.
“And, honestly, the first time you have a patient say, ‘thank you, you explained that really clearly’ ... helping just one person makes my whole degree worth it.”
On his return, Rungasamy jokes that he is going to lock all the year two and three pharmacy students in a room and tell them they have to do the Rural Health Interprofessional Programme.
“Students feel like they have to know everything about pills; but doing the Rural Health Interprofessional Programme can get students to see it’s a bit more about patients, not just the medications ... And, if you don't get out of where you've grown up, studied and then practised, you don't get those opportunities to learn that not everything is the same as where you are from and about different ways to treat people.”
The University of Otago offers similar rural placement programmes, the Tairawhiti Interprofessional Education Programme (IPE) in Gisborne and Interprofessional Education Programme (IPE) in Greymouth.
For more news from the pharmacy sector, subscribe to Pharmacy Today here