Project aims to bring cutting-edge cancer treatments to NZ
4 July 2025
Plans are under way to bring life-saving cell-based cancer treatments to patients in New Zealand.

Dr Alicia Didsbury from the University of Auckland’s Centre for Cancer Research is leading a major project aiming to provide cell and gene therapies for cancer.
The project is supported by the New Zealand Blood Service and doctors at Auckland City Hospital.
Didsbury is applying for $1.4 million for the first phase of the project, which will offer virus-specific T-cell therapy for people with blood cancers who are undergoing treatments that lower their immunity.
The aim is for the first phase to begin later this year, establishing the country’s first facility to manufacture virus-specific T-cells and a local biobank of T-cells.
From there, the plan is to launch New Zealand’s first clinical trials of cell-based treatments for a broad range of blood cancers and solid tumour cancers over the next few years.
“Cell-based therapies are the most advanced and promising treatments for cancer," says Didsbury, who is an immunologist, committee chair at the International Society for Cell and Gene Therapy, and a trustee for Ovarian Cancer Foundation NZ.
“At the moment, access to cellular therapies is extremely limited in New Zealand, so some patients go overseas and have to pay hundreds of thousands of dollars for these life-saving treatments.”
Blood-cancer patients who receive stem-cell transplants are generally given immune suppressant medication to prevent complications. This can leave patients vulnerable to potentially life-threatening viral infections.
New Zealand currently imports a small number of virus-specific T-cells, but these are expensive and not always a good match for Māori and Pacific populations, says Didsbury.
“By manufacturing virus-specific T-cells here in Auckland, we can create more affordable and better-matched therapies using local donor cells,” says Didsbury.
“For some people undergoing transplants, this could be lifesaving."
Launching a virus-specific T-cell manufacturing and treatment service in Auckland will help build the basis to launch national and international clinical trials for cell-based treatments for blood and solid tumour cancers.
The second phase of the project will make experimental treatments for multiple myeloma, melanoma, ovarian and lung cancers available in New Zealand for the first time.
“I’m a strong advocate for clinical trials in cancer care. They offer hope to patients and contribute to research that brings hope to others in the future,” says Didsbury.
Initially, the project will launch at Auckland Hospital, but Didsbury hopes clinical trials will later be offered throughout New Zealand.
For blood cancers, cell-based therapies show remarkable results. For solid tumours, cellular treatments are more experimental and have only completely cured a small percentage of patients in overseas trials.
CAR T-cell therapy is one of the most promising treatments that will be offered.
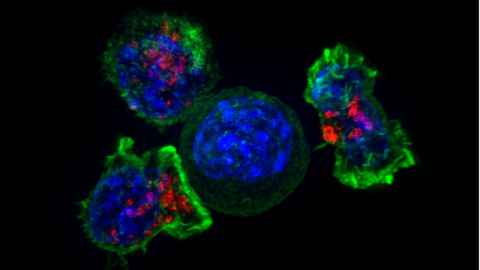
It harnesses the natural ability of T-cells – white blood cells that normally detect and kill virus-infected cells – to target cancer. In this therapy, a patient’s own T cells are collected and genetically modified in the lab to recognise and kill cancer cells. These modified cells are then infused back into the patient to fight the cancer.
CAR T-cell therapy can currently cost more than $500,000 per patient, so the project will explore affordable ways to offer these treatments within the public health system.
The new service also aims to offer other cell and gene-based cancer therapies, such as transgenic T-cell receptor therapy and tumour-infiltrating lymphocyte therapy.
Didsbury’s drive to make cancer treatments more accessible and affordable has personal roots.
“My dad passed away from cancer when I was 21 and that motivated me to pursue a career in cancer research – initially thinking I’d go into drug discovery.
“Then, in 2005, I attended a lecture from a scientist who had recently returned from Oxford who introduced me to the new idea of T-cell therapy – that was Professor Rod Dunbar. It completely changed my direction. I decided to do a PhD with him and he’s still my boss at the University of Auckland’s School of Biological Sciences,” she says.
The 46-year-old has been developing cell-based treatments for cancer for 15 years. A breakthrough treatment she helped develop for melanoma could soon be offered in clinical trials.
Media contact
Rose Davis | Research communications adviser
M: 027 568 2715
E: rose.davis@auckland.ac.nz