Psychedelics on trip back from fringe
21 April 2020
LSD and ketamine are illegal drugs. They also hold new hope for people with depression and addictions resistant to current therapy.


It seems like an experiment gone wrong: volunteers hallucinating inside an MRI machine.
In fact, University of Auckland scientists were investigating the effects of the psychedelic drug ketamine on people’s brains. Soon, another batch of volunteers in the city will take part in one of the world’s first extended studies of LSD “micro-dosing.”
The work is led by Suresh Muthukumaraswamy, an expert in brain imaging who returned to New Zealand in 2015 after taking part in ground-breaking studies of psychedelics in the United Kingdom, including producing the first images of the brain on LSD. His job title is neuro-psycho-pharmacologist and his ambition is to understand more about exactly what happens when people take mind-altering drugs, to help pave the way for a new generation of addiction and depression treatments.
New Zealand’s rising suicide toll, flood of antidepressant prescriptions, and addiction-fuelled health and crime problems underscore the need for fresh solutions. “The scale of the problem beggars belief in some ways,” he says, citing a suicide toll that jumped to a record 685 in the year to June 2019.
Muthukumaraswamy’s work is part of a renaissance in psychedelic research this century after a moral panic in the 1960s mostly halted investigations into medical applications for the drugs.
These days, a leading theory is that psychedelics diminish activity in the “default mode network,” an area of the brain involved in maintaining a sense of self and engaging in self-reflection.
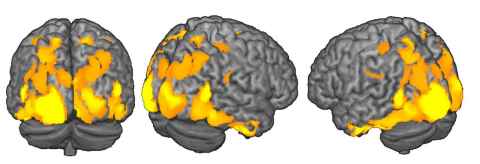
This is where addicts or people suffering from depression would ruminate on self-defeating stories of their lives. Scientists speculate that temporarily limiting the default mode network allows for the spiritual experience known as “ego dissolution,” engendering a sense of connectedness with the world, and potentially helping addicts and the depressed to break free from repetitive patterns of thinking.
For Muthakumaraswamy and Rachael Sumner, the research fellow who ran the ketamine study, one key avenue of exploration is the theory that psychedelics enhance neural plasticity, the ability of brain cells to form new connections. That ability may be diminished in people who suffer from depression or are trapped in repetitive behaviours such as addiction or obsessive-compulsive disorder.
In the ketamine study, conducted between 2016 and 2018, 30 people with treatment-resistant depression were infused intravenously with the drug, then scanned in an MRI machine.
Hallucinations including being in control of a spaceship in a Star Wars setting; losing all sense of space and time; and “floating outside of my body… it felt like my hands were on backwards.”
Three or four hours after taking ketamine, when the psychedelic effects had faded, and having rested and had lunch, the volunteers were wired up to an electroencephalography (EEG) machine to monitor their brains as they focused on a red dot on a screen as black and white images flashed past.
First for humans
This simple task allowed the scientists to witness “long-term potentiation”, the term for a strengthening of synapses in response to a stimulus, which indicates increased neural plasticity. The effect had been seen previously in rodents on ketamine, but this was a first for humans.
Most of the volunteers’ symptoms of depression fell by 50 percent or more within a day, but the improvements faded after a week or so. Those results were typical for a drug that has stoked excitement around the world because of its rapid antidepressant properties.
In some cases, volunteers gained hope simply from knowing they were capable of feeling happier. One person reported becoming “a functional human being” for the first time, free for a week or two from guilt, overwhelming dread and a constant sense that something was wrong.
Ketamine is a good illustration of how a drug with a bad reputation has the potential to offer remarkable medical gains. Nicknamed “Special K,” the human and animal tranquiliser and party drug can trigger a dissociative state termed a “K-hole.” It’s a Class C illegal drug in New Zealand alongside the likes of cannabis and codeine.

Close to remission
“There’s all this stigma about it in society,” Muthukumaraswamy says, “But if you just take a step back, and think about it from a purely scientific perspective – you’ve got patients who have been depressed for 20 years. You can give them a single dose of ketamine and the next day their depression will be close to remission.”
The pending LSD study is another brush with a bad reputation. New Zealand law classifies the drug as a Class A illicit substance, alongside magic mushrooms (psilocybin), heroin, cocaine and methamphetamine, with manufacturers or suppliers risking sentences of life imprisonment.
For Muthukumaraswamy the drug’s status adds complications to his experiment, with extra scrutiny from regulators, special approvals required to source the drug from a manufacturer in the UK, and research funding likely harder to source. Psychedelic studies also attract media interest, along with unwanted efforts by recreational drug users to get involved.
In the pending experiment, 40 healthy, male volunteers will self-administer a low sub-psychedelic dose in an oral solution, perhaps a tenth of the strength of an acid tab sold on the street, at home every fourth morning while continuing to go about their regular daily routines.
Made famous by Silicon Valley entrepreneurs and promoted by a 2011 protocol by US psychedelic researcher James Fadiman, LSD micro-dosing has gone global, with users in countries including New Zealand claiming improvements in mood, creativity, focus and cognition. Unlike the underground drug users, the Auckland volunteers will face rigorous oversight, from daily questionnaires to periodic laboratory tests where electrodes on the scalp will measure how their brains adapt to simple sensory tasks, again checking on neural plasticity effects.
"Taking part will be a big undertaking, it’s not a holiday,” the scientist says. "We’re going to be prodding them and probing them, making them do tasks, sticking electrodes all over them and putting them in scanners. We’ll be studying them for three months and they’ll have to come into our lab for pretty much five full days.”
In what’s called a two-by-two crossover design, half of the volunteers will start on placebo and half will start on LSD, with the two groups swapped midway through the exercise. The test subjects will be all male to avoid menstrual-cycle effects on measures of mood and function.
“Taking part will be a big undertaking, it’s not a holiday.”
Back to the future
Delving into the potential of psychedelics is a back-to-the-future exercise. “It’s important to know the historical context,” says Muthukumaraswamy. “It was very mainstream in psychology in the 1950s and 1960s, the study of these drugs.”
Lysergic acid diethylamide was first synthesized by Swiss chemist Albert Hoffman in 1938, who discovered its psychedelic effects five years later. An article in Life magazine in 1957 brought psilocybin or “magic mushrooms” to public attention. Alcoholics Anonymous founder Bill Wilson experimented with LSD and six clinical trials published in the late 1960s and early 1970s indicated the drug had potential as a treatment for alcoholism, according to a retrospective analysis. US Senator Robert Kennedy spoke of the promise of psychedelics.
In New Zealand, LSD’s one-time status as a therapeutic tool is revealed on the shelves of medical libraries in the pages of the October, 1966 edition of the New Zealand Medical Journal. A Christchurch psychiatrist, David Livingstone, contributed “Some General Observations on the Usefulness of Lysergic Acid in Psychiatry” after treating 55 patients in 131 sessions of seven to eight hours each.
He said LSD spurred “psychotherapeutic flexibility and responsiveness through the freeing up of rigid psychological defence mechanisms,” with an increasing number of psychiatrists in New Zealand and Australia adding the drug to their therapeutic toolkits. But the psychiatrist’s article came just as a moral panic was mounting.

Medical use halted
While psychedelic drugs were associated with a flowering of creativity, as illustrated by trippy counter-cultural artworks and the LSD-influenced music of the Beatles’ album Revolver, the US media increasingly focused on tales of bad trips and drug-fuelled mayhem. “LSD: The Exploding Threat of the Mind Drug That Got Out of Control,” Life magazine’s cover blared in 1966. By 1967, LSD was illegal in New Zealand, and research into medical uses ground to a halt around the world as US regulators cracked down and a company manufacturing the drug, Sandoz, withdrew supplies that had been free for medical experiments.
Interest in psychedelics flowered again this century, with studies at institutions such as New York University, Johns Hopkins University in Baltimore and Imperial College in London. Experiments pointed to the potential for psilocybin, the active ingredient in “magic mushrooms,” to help smokers quit and to aid cancer patients wrestling with anxiety and depression. MDMA, or ecstasy, featured in experimental treatments for post-traumatic stress disorder. Ketamine showed its powerful antidepressant properties.
Muthukumaraswamy, a graduate of the University of Auckland, played a key role in ground-breaking UK studies involving two leading psychedelic researchers, former UK government drugs adviser David Nutt and Robert Carhart-Harris, both of Imperial College, when he worked in Wales at the Cardiff University Brian Research Imaging Centre.
One study to grab headlines around the world in 2016 showed the first – and very colourful – images of brains on LSD. This study seemed to show increased communication between regions of the brain that were normally isolated from each other.
Antidepressants are taken by more than 400,000 New Zealanders.
Fresh approach needed
The need for fresh approaches to mental illness and addiction is illustrated by some startling New Zealand numbers. Antidepressants are taken by more than 400,000 people. As many as 20,000 people attempt to kill themselves each year, according to a 2018 report on mental health and addiction, while an overall suicide rate of 13.93 per 100,000 people is doubled for Māori.
The youth suicide rate is among the worst in economically developed nations. The 2018 government inquiry into mental health and addiction pointed to a society awash in alcohol, with widespread hazardous drinking fuelling crime and health problems.
Methamphetamine abuse rages. The potential for psychedelics is to come at mental illness and addiction from a different angle than existing treatments such as Naltrexone, which blocks opioid receptors in the brains of addicted alcohol or opiate users, or methadone, a substitute for heroin which can itself be addictive, or selective serotonin uptake inhibitors (SSRIs), which treat depression by increasing levels of serotonin in the brain.
The experiments by the Auckland scientists come with a health warning: don’t try this at home. The volunteers taking part in research are closely monitored to mitigate adverse reactions to the psychedelics – and can also be sure of exactly what drug and dose they’re getting, unlike a street user.
Story by Paul Panckhurst
The Challenge is a continuing series from the University of Auckland about
how our researchers are helping to tackle some of the world's biggest challenges.
To republish this article please contact: gilbert.wong@auckland.ac.nz