Human trial brings hope for millions of gut sufferers
05 March 2024
A world-leading device developed by University of Auckland researchers to measure faulty gut electrical signals has passed a major milestone

World-leading medical technology which could allow doctors to diagnose hard-to-identify stomach complaints without invasive surgery has passed a critical hurdle – a successful human study.
The endoscopic mapping device, developed over more than a decade by scientists at the Auckland Bioengineering Institute, consists of an inflatable sphere covered in sensors, delivered down the oesophagus and able to measure electrical activity in the gut.
In the same way abnormal heart electrical signals can cause serious heart problems, so research has found faulty bioelectric gut waves can lead to stomach pain, nausea, vomiting and bloating.
But often doctors can’t find out what the problem is. That’s because gut electrics aren’t nearly as strong or as easily measured as heart waves; without surgery it’s hard to know if someone has a so-called `dysrhythmic’ gut – and if so, where the problem is.
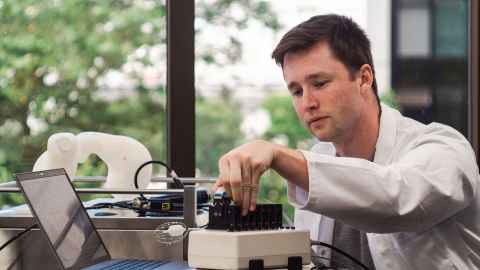
Enter University of Auckland gastrointestinal researcher Dr Tim Angeli-Gordon, the head of the team which has developed the endoscopic sensor device.
“This is a critical step, taking us from engineering and pre-clinical work to real patients. “It’s very difficult to do, but this is the dream; the pinnacle of bioengineering.”

A paper published this week in the highly-regarded journal Device details the results of the initial study into 13 patients. Additional data has since been collected from 35 patients in Auckland and Christchurch, Angeli-Gordon says.
“We’re still analysing those data but it looks very promising.”
Peter Tremain, a postgraduate researcher and the lead author of the paper, says the next step is to use the data from the two human clinical studies to improve the design of the device.
In particular, he wants to improve filtering of the electrical signal, so clinicians can isolate gut signals from competing `noise’.
“The body produces a lot of random electrical confusion,” Tremain says. And the problem is that stomach signals, in comparison with those from the heart, are much closer in amplitude to this random noise.
Meanwhile, outside vibrations, like vibrations from equipment, or people walking around, can also produce noise in the electrical signals, Tremain says.
“As part of this paper, we’ve managed to extract stomach signals from that noise; now we want to hone this even more.”
Angeli-Gordon says human studies are the most recent stage in a decades-long process, building on the initial discovery in the early 1900s that the gut, like the heart, was governed by electrical signals. More recently, scientists like Angeli-Gordon have been studying faulty gut electrics.
The trouble with early studies was that, because of the weak stomach signals, diagnosis of gut dysrhythmia involved open surgery and putting electrodes on the outside of the stomach.
“We realised if we ever wanted to apply these techniques to a larger patient group we needed minimally-invasive options,” Angeli-Gordon says.
In 2022, ABI spin-off company Alimetry got the green light from the US Food and Drug Administration for the gut version of an electrocardiogram (ECG) – a high-resolution gastric mapping tool which straps onto the outside of your abdomen and can tell doctors whether someone’s electric signals are normal or not.
The gastric Alimetry system is available in the US, UK and New Zealand.
We realised if we ever wanted to apply these techniques to a larger patient group we needed minimally-invasive options.
The endoscopic sensor system which is the subject of the new research paper takes the diagnosis one step further – aiming to give clinicians a clearer picture of exactly where the electrical signals are misfiring.
“It initially allows us to record if the bioelectrical activity is abnormal; it can be a real relief to patients to have a definitive measurement of what is wrong with their gut. Then we look at how we can correct that,” Angeli-Gordon says.
A different group at the Auckland Bioengineering Institute, also led by Dr Angeli-Gordon, is exploring whether ablation – the careful burning technique used in the heart to block irregular electrical signals – could be used endoscopically to correct problems in the gut.
Early test results in animals are very encouraging, and the team is continuing to progress that technology towards being used in clinic too, Angeli-Gordon says.
Patients can sometimes struggle for years to get a diagnosis. Some even get referred to psychiatrists because their doctors eventually conclude their symptoms are all in their heads.
Angeli-Gordon estimates about a third of patients who go to their doctor with gut-related symptoms have some sort of electrical abnormality. That equates to millions of sufferers worldwide.
Research has shown ‘functional dyspepsia’ – stomach problems which appear to have no structural rationale – afflicts between five and 11 percent of the population.
Patients can sometimes struggle for years to get a diagnosis, Angeli-Gordon says. Some even get referred to psychiatrists because their doctors eventually conclude their symptoms are all in their heads.
For patients and clinicians, accurate diagnosis and treatment can’t come soon enough, although Angeli-Gordon reckons it could be another five years before the endoscopic device is widely available in hospitals around the world.
The human studies are an important first step.
“We are also looking at options for commercialisation – figuring out how we can best progress this promising technology,” he says.
The research so far has been funded in part from a Rutherford Discovery Fellowship from the Royal Society Te Apārangi, but that comes to an end this year. An additional year of support has been secured from Te Tītoki Mataora MedTech Research Translator, enabling the team to continue to advance this technology and explore options for longer-term support.
Listen to Dr Tim Angeli-Gordon at Raising the Bar 2023: Secrets of the Electric Stomach
Media contact
Nikki Mandow | Media adviser
M: 021 174 3142
E: nikki.mandow@auckland.ac.nz